Ulcerative Colitis
"The cause of ulcerative colitis is not known, although there is a genetic predisposition that causes first-degree relatives of affected people to have a 4 to 20 times greater risk of suffering it".
DR. Mª TERESA BETÉS
SPECIALIST. DIGESTIVE DEPARTMENT

Ulcerative colitis is a chronic inflammatory affectation of the digestive tract that evolves in a recurrent way with outbreaks.
Ulcerative colitis affects exclusively the colon, being the most frequent location in the rectum. It can present manifestations outside the digestive system as in joints, skin, liver, eyes...
There is an increased risk of colon cancer, fundamentally, and this risk increases progressively from 10 years after the diagnosis of the disease.
The quality of life between the outbreaks of this disease is good and during the times in which there are symptoms it is important to have the supervision of your doctor.
For this reason it is important the precocious diagnosis recommending an annual endoscopic pursuit from the 10 years of the diagnosis with taking of multiple biopsies if suspicious zones and biopsies of those elevated or narrow zones do not exist.

What are the symptoms of Ulcerative Colitis?
The symptoms depend on the anatomical location and the severity of the inflammation.
In ulcerative colitis the involvement at the rectal level is the most common symptom being the expulsion of blood through the rectum usually accompanied by increased number of stools.
Abdominal pain can be associated more or less diffuse that improves initially with defecation. There may be fever and weight loss depending on the severity, duration and location of the outbreak.
The most common symptoms are:
- Expulsion of blood from the rectum.
- Abdominal pain.
- Fever.
- Loss of weight.
Do you have any of these symptoms?
You may have ulcerative colitis
What are the causes of Ulcerative Colitis?
The cause of this disease is not known. There are many hypotheses, but the most current one is that there is an alteration in the immune system to food or bacterial antigens.
Other theories establish an infectious process as the trigger of the disease, with several germs being involved. Everything suggests that there are multiple factors involved in the origin of the disease.
What is the prognosis of Ulcerative Colitis?
Since no drug is available at the moment that will prevent recurrences, the prognosis is uncertain and individual.
The prognosis is generally related to the time of evolution of the disease since the diagnosis, the extension of the disease, the severity of the outbreaks, the existence or not of complications and the history of surgical treatment.
A special mention is made of the possibility of malignancy in the course of this disease. There is an increased risk of tumor, especially of the colon, compared to the general population. This risk increases progressively from 10 years after the diagnosis of the disease.
How is Ulcerative Colitis diagnosed?
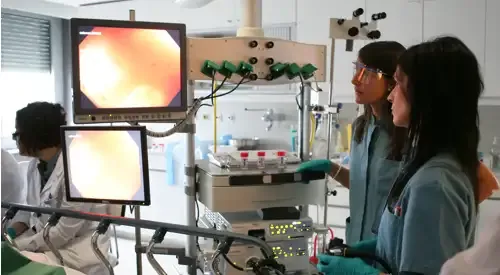
The diagnosis of ulcerative colitis is made with clinical suspicion and compatible radiological, endoscopic and histological (biopsy) findings.
Early diagnosis is important, recommending an annual endoscopic follow-up from 10 years after diagnosis with multiple biopsies if there are no suspicious areas and biopsies of those areas raised or narrowed. Depending on the result of the study of the samples, the attitude to be followed will be decided.
Radiological studies (CT, ultrasound, intestinal transit) will show the extent of the lesions and possible complications such as stenosis (narrowing), abscesses, fistulas, etc.
The scan with marked leukocytes can allow the extension of the inflammation of the disease to be assessed, as well as to distinguish whether the areas with difficulty in passing are due to inflammation or to the scar or fibrotic component.
At the moment of the appearance of the symptoms, it should be differentiated from other entities with outbreaks of diarrhea, bloody abdominal pain and/or fever (colitis of infectious origin, secondary to antibiotic intake, intestinal tuberculosis, acute appendicitis, colitis secondary to radiotherapy or of vascular origin...).
How is Ulcerative Colitis treated?
Steroids, 5-ASA, antibiotics, immunosuppressants or methotrexate can be used in outbreaks. There are other newer treatments based on the alteration of the immune system such as anti-TNF monoclonal antibodies (such as infliximab, the first one authorized). These last ones should be applied in reference centers with the aim of allowing later studies to extend or not the current indications.
There are other treatments, such as granulocytopheresis, whose objective is to absorb in an apheresis column the blood cells responsible for the perpetuation of inflammation. A weekly session is performed, during five weeks. In those patients who present clinical response, a "reminder" can be considered every 6 weeks.
In the remission phase, one should try to withdraw, although this is not always possible, the intake of steroids, leaving the maintenance 5-ASA. The pharmacological treatment must be accompanied by correct renutrition of the patient.
Where do we treat it?
IN NAVARRE AND MADRID
The Department of Digestive
of the Clínica Universidad de Navarra
The Digestive Department of the Clinica Universidad de Navarra is composed of a multidisciplinary team of specialists who are experts in the diagnosis and treatment of diseases of the digestive tract.
Our objective is that each diagnosis be carefully established and the treatment plan adjusted to each patient.

Why at the Clinica?
- Medical specialists who are national references.
- Specialized nursing team.
- Endoscopy Unit and High Risk Digestive Tumor Prevention and Consultation Unit to offer the best care to our patients.















