Vertebral infections
"Early diagnosis, and starting antibiotic treatment as soon as possible, increases the possibility of cure and avoids major complications".
DR. VICTOR RODRIGO PARADELLS
SPECIALIST. NEUROSURGERY DEPARTMENT
Spinal infection occurs when a microorganism invades the spine.
- Epidural or subdural empyema. An empyema is an infection located in a space of a cavity. In this case it can be in the epidural space or in the subdural space.
- Vertebral osteomyelitis or infectious spondylitis An abscess is an organized infection in a tissue. When it affects the bone, that is, the vertebra, it is called vertebral osteomyelitis or infectious spondylitis.
Without the infection affecting only the intervertebral disc, it is called infectious disc disease. If it is mixed (disc and vertebra), it is called infectious spondylitis.
If the infection affects the membranes that cover the nervous system, meningitis will develop.
The thoracic level is the most frequently affected (50%) followed by the lumbar (35%) and cervical (15%). Often empyema and dyscites or osteomyelitis coexist.

What are the symptoms of a spinal infection?
Vertebral infection appears by three ways of dissemination of the microorganisms: by hematogenous route, direct external inoculation and by contiguity from neighboring tissues.
The infection of the spine can cause constant pain, which worsens at night and with changes in position, wandering and activity.
This pain may radiate to the chest or abdomen.
When it affects cervical spaces it can cause dysphagia and/or torticollis.
If there is a neurological deficit, hypesthesia (decreased sensitivity), numbness and cramps may appear in the affected extremity.
The most common symptoms are:
- Local, non-specific and moderate pain.
- Fever.
- General malaise and general fatigue.
- Neurological alterations.
Do you have any of these symptoms?
You may have a spinal infection
What are the causes of a spinal infection?
The origin of the infection can be iatrogenic (surgeries or punctures) or by hematogenous dissemination and sometimes it is even impossible to discern the origin of the pathogen (up to 50% in some series).
Today they are becoming less frequent as advances in surgical asepsis and antibiotherapy have significantly reduced these infections.
The Staphylococco aureus is the most frequently observed germ (>50%). Tuberculosis (Pott's disease) and fungal infections, which are very rare in immunocompetent individuals, should be suspected in immunocompromised patients or patients addicted to parenteral drugs (ADVP).
What are the risk factors?
There are some factors that may favor the appearance of a spinal infection:
Diabetes mellitus, alcoholism, penetrating trauma, previous surgical procedure, advanced age, obesity, malnutrition, immunosuppression or immunodulation (corticotherapy, HIV/AIDS, transplants, etc.), drug addiction, significant medical comorbidity, poor condition of the patient, hemodialysis, etc.
How is a spinal infection diagnosed?
Laboratory tests (globular sedimentation rate (ESR), C-reactive protein (CRP), procalcitonin, leukocyte formula etc.) These are indispensable parameters for the control of this type of disease.
The simple radiological study provides information on the chronological changes in the bone, but is not sufficient for an assessment of the acute-subacute phase of the disease; however, a dynamic X-ray to assess the stability of the vertebrae depending on how much it has affected the vertebrae are also of great importance.
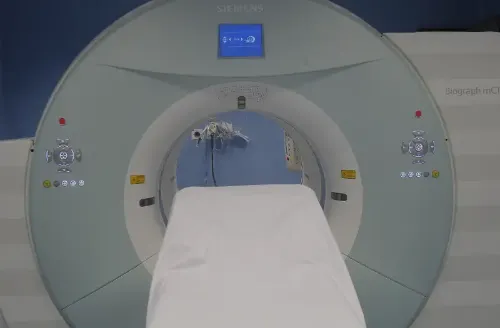
The magnetic resonance (soft parts) and the scanner or CT (bone elements) are the reference tests for an adequate and effective study of the infection.
Nuclear medicine tests can also help in doubtful cases. These are the scan with marked leukocytes or with Gallium/Technetium, the SPECT-CT and the PET-CT.
The definitive study for the diagnosis of an infection is a biopsy to obtain samples for the culture of the pathogen to be treated. It can be carried out in a surgical act or in a percutaneous way guided with CT.
How is a spinal infection treated?
The treatment for any of these infections is intravenous antibiotherapy. If we know the pathogen that has caused the infection, you will be given targeted antibiotherapy. If the origin of the infection is still unknown, broad-spectrum antibiotics will be used.
If the empyema or abscess produces a clear compression on nerve structures, surgery is indicated to relieve pressure on the affected area.
If, due to bone destruction, there is vertebral instability, stabilization surgery may be indicated, since this is often a consequence of the infection, leading to greater pain problems for the patient.
In a post-surgical infectious discitis, the usual treatment is empirical intravenous antibiotherapy, rest and a lumbar or dorsal-lumbar orthosis.
Where do we treat it?
IN NAVARRE AND MADRID
The Department of Neurosurgery
at the Clínica Universidad de Navarra
The Neurosurgery Department has specialists with a great deal of experience in care and research and the most advanced technology.
We are the first Spanish center that incorporates high field intraoperative magnetic resonance (3T). This allows the maximum precision and control in cranial surgery.
We are the Spanish medical center with the most experience in Parkinson's surgery by means of deep brain stimulation. We have the latest technology with localized ultrasound (HIFU) and extensive experience in treating essential tremor and Parkinson's disease without an incision.
Treatments we perform
- Alterations in the circulation of the cerebrospinal fluid
- Infusion Pumps
- Epilepsy Surgery
- Deep brain stimulation
- HIFU, high intensity ultrasound
- Trigeminal Neuralgia
- Pediatric Neurosurgery
- Neuronavigation of the spine
- Spine Pathology
- Brain Tumors
- Pituitary Tumors

Why in Navarre?
- The first Spanish center with a high field intraoperative magnetic resonance (3T).
- Precision and minimally invasive surgery.
- Experts in the use of HIFU for the treatment of tremor.




